Lupine Publishers | Journal of Health Research and Reviews
Short Communication
Despite all of the available diagnostic and treatment modalities
atherosclerosis remains one of the most common healthcare
problems worldwide with an estimated annual mortality rate of
approximately 17,5 million cases [1]. In most cases acute coronary
syndrome (ACS) appears to be linked to atherosclerotic lesion
associated thrombosis of a vessel [2]. In the situation, when patients
come to the interventional cardiology unit with a confirmed
diagnosis of ACS: myocardial infarction, a so-called culprit lesion
can be identified and treated according to international guidelines.
However, alongside the lesions, that are obviously causing an
impairment of a blood perfusion in a certain segment of the
myocardium or have already destabilized causing acute thrombosis,
some other form of entity can frequently be seen. These are called
non – culprit lesions. Even though their appearance in an orifice
of a vessel is regarded by most surgeons as a “bad omen”, the
international community is still puzzled and unsure, if these lesions
are to be treated. And even if they are, the specialists cannot yet be
sure, what type of an intervention is preferable. This problem arises
from several premises, including the following:
I. The non – culprit vulnerable plaque destabilization is a
complex phenomenon. Not only the mechanical properties and
structural integrity of the plaque define the further events,
but the mechanical forces [3-5], that affect the plaque and are
being transduces by blood flow, a non-Newtonian fluid, whose
properties might be affected in a large variety of conditions.
Apparently, the hemostasis must be accessed prior to drawing
the right decision in patient’s follow – up tactics. But exact
parameters are yet to be determined [6].
II. The non – culprit vulnerable plaque destabilization
does not always cause an ACS [7]. Some specialists imply that
assessment of blood properties and structural characteristics
of the plaque are not enough. Apparently, the state of a
myocardium must also be assessed.
III. Not all vulnerable plaques are equal, and the risks of
destabilization accompanied by MACE vary depending on
the plaque localization [8]. This statement appears to be
obvious. Most surgeons would have guessed this without any
researches: the more approximate position in a coronary artery
clearly indicates a higher chance of an unfavorable outcome.
However, what might be not so apparent, the different segments
of coronary arteries’ do not react to sheer-stress in a uniform
manner [9]. This is almost impossible to assess in real clinical
practice but is a good thing to bear in mind.
One must put a lot of effort into the diagnostic procedures, in
order to understand the whole situation. Simultaneously we do not
know what kind of a medication must be used in every situation.
A lot of effort has been put recently into finding a preferable drug
for stabilization of a vulnerable plaque. Different approaches were
used. Considering the trails REVERSAL, SATURN, ASTEROID and
most importantly YELLOW, the conventional statins are still a
medication of choice for the most patients with vulnerable plaques.
Other drugs were introduced recently, including ivabradine [10],
grelin [11], canakinumab [12]. Most of these approaches are still
in early development, but it is clear now, that the lack of preventive
conservative treatment is a risk factor for any manipulation [13],
that is to be performed upon a vulnerable plaque.
Some cardiologists imply that more aggressive invasive
techniques should be prioritized. We possess only scarce data.
PRAMI trial indicates, that stenting any lesion, that is even less
than 50% might be beneficial [14]. The CvLPRIP trial has mostly
confirmed the findings of PRAMI [15]. Interesting results were
obtained by Dai et al [16] they were able to demonstrate, that routine
stenting of all lesions leads to lower rates of death, secondary ACS.
MACCE were lower: RR (HR) 0.35 [95% CI 0.18 – 0.69]. Additional
factors listed above might contribute to drawing a right decision in
different situations.
The problem with invasive procedures extends beyond that:
I. The risks of stent - thrombosis are unacceptable in
endovascular plaque stabilization. This in turn requires at
least using an extremely precise tool, that has only limited
contact with endothelial cells, that have not yet succumbed
to pathological process. Extensive damage frequently leads
to neointimal hyperplasia, neoatherosclerosis and stent
thrombosis. Considering all things stated, we suppose, that
only truncated stents might be used for vulnerable plaque
stabilization.
II. The usage of truncated stents requires a fairly good level
of precision, that most devices nowadays are still unable to
provide.
III. The risks of bleeding are also high, because a person is
forced to take a variety of anticoagulants for a prolonged period
after the procedure. The bigger the time interval, the bigger the
chances of a major bleeding. Therefore, there is a question to be
asked: what if the biodegradable stents, that did not legitimately
receive much attention due to the known issues and inability
to compete with DES in terms of conventional stenting, can be
used in this situation.
IV. The risks of periprocedural myocardial infarction [17]
are dependent on structural properties of the plaque. High
lipid burden and large lipid core are mostly responsible for this
adverse event [18]. This cannot be manipulated by the means
of surgical instruments and is a single reason for carefully
assessing the situation using different diagnostic techniques.
V. It is economically ineffective to create a separate device
for treatment of vulnerable plaques only.
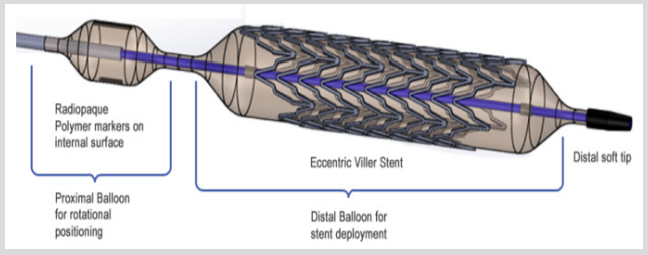
VI. Bearing in mind all the concerns stated, we decided
to come up with a new device that can be used in many
different fields but is also capable to satisfy all the precautions
involved in vulnerable plaque endovascular stabilization. The
throughout description of the basics of this over the wire stent
delivery systems (SDS) construction is not however the goal
of this article. All the information can be found in our patent
here: US 20100070014 A1 published in 2010. The project
is in early development and we do not encourage a reader to
buy it. Therefore, this article is not a commercial, but a call to
international specialists, that would probably find this topic
interesting to discuss. The basic structure of the SDSs distal
shaft is shown below (Figure 1).
Figure 1.
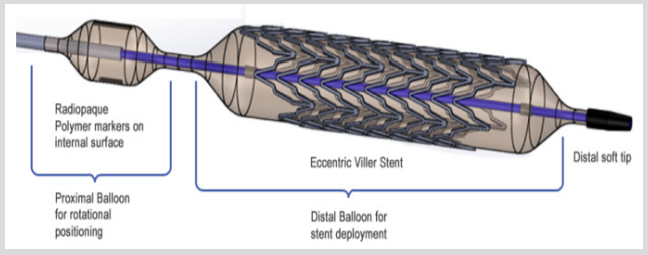
Such SDS works in following order. Both balloons are connected
consecutively to the compressor, but radiopaque label bearing
balloon is more compliant and expands in the first place allowing the
precise positioning of asymmetrical truncated stent in the orifice of
the vessel. By applying sufficient force, the operator can ensure that
the stent is in position, meanwhile, by applying additional pressure,
can start the expansion of the second stent- bearing balloon. After
the implantation is complete the SDS is removed at once. We are
currently developing new biodegradable stents and will test the
whole system on a swine model in several months.
For more Lupine Publishers Research and Reviews on Healthcare Open Access Journal Articles:
https://lupine-publishers-research.blogspot.com/