Abstract
Background: In the era of super bugs, there is a need to
monitor antibiotic resistance patterns. Due to the emergence of
antimicrobial resistance worldwide, local antibiotic resistance patterns
should be monitored periodically to alert early intervention.
This audit was conducted to analyse the antibiotic resistance patterns
among the gonococcal urethritis cases that presented to the
Genitourinary Medicine (GUM) Clinic, Hospital Kuala Lumpur (HKL),
Malaysia.
Methodology: This is a retrospective study on the antibiotic
resistance patterns based on 370 culture positive gonorrhoea
obtained from urethral swab samples sent between 2011 and 2015.
Antimicrobial susceptibility testing by standard disc diffusion
method was performed to detect sensitivity to penicillin, tetracycline,
ciprofloxacin, cefuroxime, azithromycin and ceftriaxone. All
data was obtained from microbiology report and patient records.
Results: A total of 370 positive culture isolates of
N.gonorrhoeae (new and recurrent cases) from 2011 to 2015 were reviewed.
Highest level of resistance detected was to azithromycin (100%, 64/64)
followed by tetracycline (82.8%, 293/354). Resistance
to penicillin was noted in 60.9% (224/368) of all isolates. Both
penicillin and tetracycline showed a decreasing resistance trend
from 2011-2015. The fourth commonest antibiotic resistance was to
ciprofloxacin at 46.5% (158/340). Cephalosporins tested were
cefuroxime and ceftriaxone, which showed resistance rates of 2.7%
(6/219) and 0.8% (3/364), respectively.
Conclusion: The complete resistance to azithromycin is
alarming since it is a common antibiotic used to treat urethral
discharge
using the syndromic approach. Penicillin and tetracycline resistance
remain high in Malaysia and other Western Pacific countries.
The current first line antibiotic for treating gonorrhoea in GUM Clinic,
HKL is ceftriaxone. Clinicians should be aware of the newly
discovered increase in resistance observed to ceftriaxone.
Keywords: Neisseria gonorrhoeae; Gonorrhoea; Antibiotic Resistance
Introduction
The last decade has seen Neisseria gonorrhoeae emerging
as a true superbug, bringing.com closer to a time of untreatable
gonorrhoea. This diplococcal microbe is able to recombine its
genes and invade the immune system through antigenic variation.
It is also naturally competent to acquire new deoxyribonucleic
acid (DNA), enabling N. gonorrhoeae to spread new genes,
disguise itself with different surface proteins, and prevent the
development of immunological memory an ability that has led to
antibiotic resistance and has made vaccine development difficult.
Gonorrhea is a debilitating disease, which was responsible for an
estimated 445,000 years lived with disability in 2015, according
to a systemic analysis for the Global Burden of Disease Study [1].
Patients infected with N.gonorrhoeae are known to present with
urethral discharge, malaise and symptoms that may suggest a
urinary tract infection. Nevertheless, urogenital gonorrhea may be
asymptomatic in 40% of men and often manifests as urethritis [2,3].
Unfortunately, it is also asymptomatic in more than half of women
[4]. In men, untreated urethral infection can lead to epididymitis,
reduced fertility, and cause urethral strictures. In women, if present,
symptoms are non specific and include abnormal vaginal discharge,
dysuria, lower abdominal discomfort, and dyspareunia. The lack
of discernible symptoms results in unrecognized and untreated
infections, which can lead to serious complications [5]. Overall,
10%-20% of female patients develop pelvic inflammatory disease
(PID) and, consequently, are at risk for infertility [6]. Pregnancy
complications associated with gonorrhea include chorioamnionitis,
premature rupture of membranes, preterm birth, ectopic
pregnancies, and spontaneous abortions [5,7,8]. Infants of mothers
with gonococcal infection can be infected at delivery, resulting in
neonatal conjunctivitis (ophthalmia neonatorum). Such untreated
conjunctivitis may lead to scarring and blindness.
Extragenital infections are common in both sexes and frequently
occur in the absence of urogenital infection [9,10]. Rectal infections
are usually asymptomatic but can manifest as rectal and anal pain
or discharge. Pharyngeal infections are mostly asymptomatic, but
mild sore throat and pharyngitis may occur. Although bacterial
concentrations are generally lower than in other infection sites, the
pharynx is thought to be a favourable site for resistance emergence
due to acquisition of resistance traits from commensal Neisseria
spp [11]. Disseminated gonococcal infections with gonococcal
arthritis also occur. Because they are frequently asymptomatic,
extragenital infections often remain untreated, despite their key
role in disease transmission. Co-infection with other major Sexually
Transmitted Infections (STIs) HIV, Herpes simplex virus, Chlamydia
trachomatis, Mycoplasma genitalium, and Treponema pallidum
are common and may result in synergistic effects on transmission
and disease severity. Attempts to treat and control gonorrhoea are
compromised by the emergence and spread of antibiotic resistant
N.gonorrhoeae. Antibiotic resistance pattern vary between
different geographical areas. It is therefore important to know the
local antibiotic resistance pattern, so that appropriate treatment
can be instituted. In Malaysia, Kanamycin was used as the first line
antibiotic to treat gonorrhoea during the early 1970’s and 80’s,
which was subsequently changed to Spectinomycin, followed by
Ceftriaxone since the early 1990’s [12] There are many surveillance
programmes on antibiotic resistance patterns of N.gonorrhoeae
such as GRASP (Gonococcal Resistance to Antimicrobial Surveilance
Programme), that is based in London, UK, and WHO (World Health
Organization) Antimicrobial Surveilance Programme [13,14].
Materials and Methods
All patients with positive culture for gonorrhoea, who attended
the GUM clinic in HKL between 2011-2015, were included in
this study. Antimicrobial susceptibility testing by standard disc
diffusion method was performed to detect sensitivity to Penicillin,
Tetracycline, Ciprofloxacin, Cefuroxime, Azithromycin and
Ceftriaxone. Data was obtained from patient records and formal
microbiology laboratory results.
Results
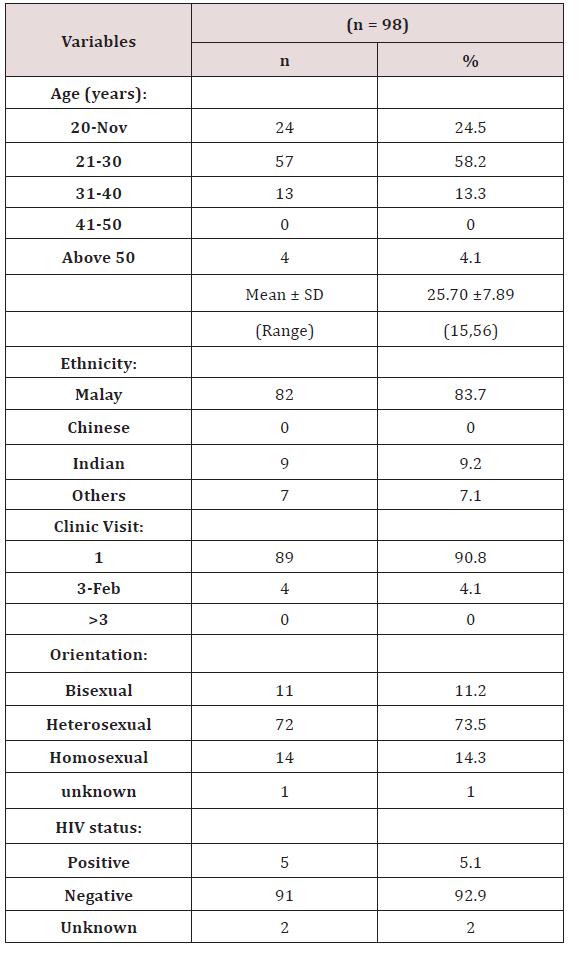
370 positive culture isolates of N.gonorrhoeae from patients
seen in 2011-2015 were included in this study. Most of the
data were obtained from the microbiology laboratory results.
Demographic data was available for 98 patients only. More than
half of the patients (58.2%) were between 21-30 years old. Most
patients were Malay (83.7%), followed by Indian (9.2%). Overall,
the heterosexually orientated patients represented about 73% of
gonococcal urethritis cases. Majority of cases (92%) tested negative
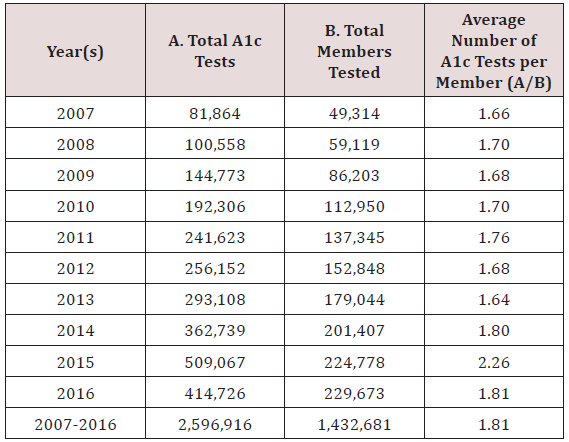
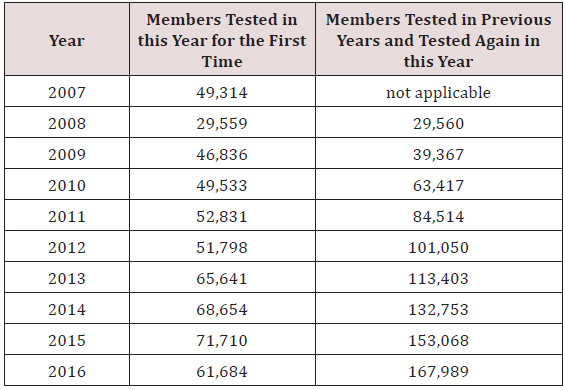
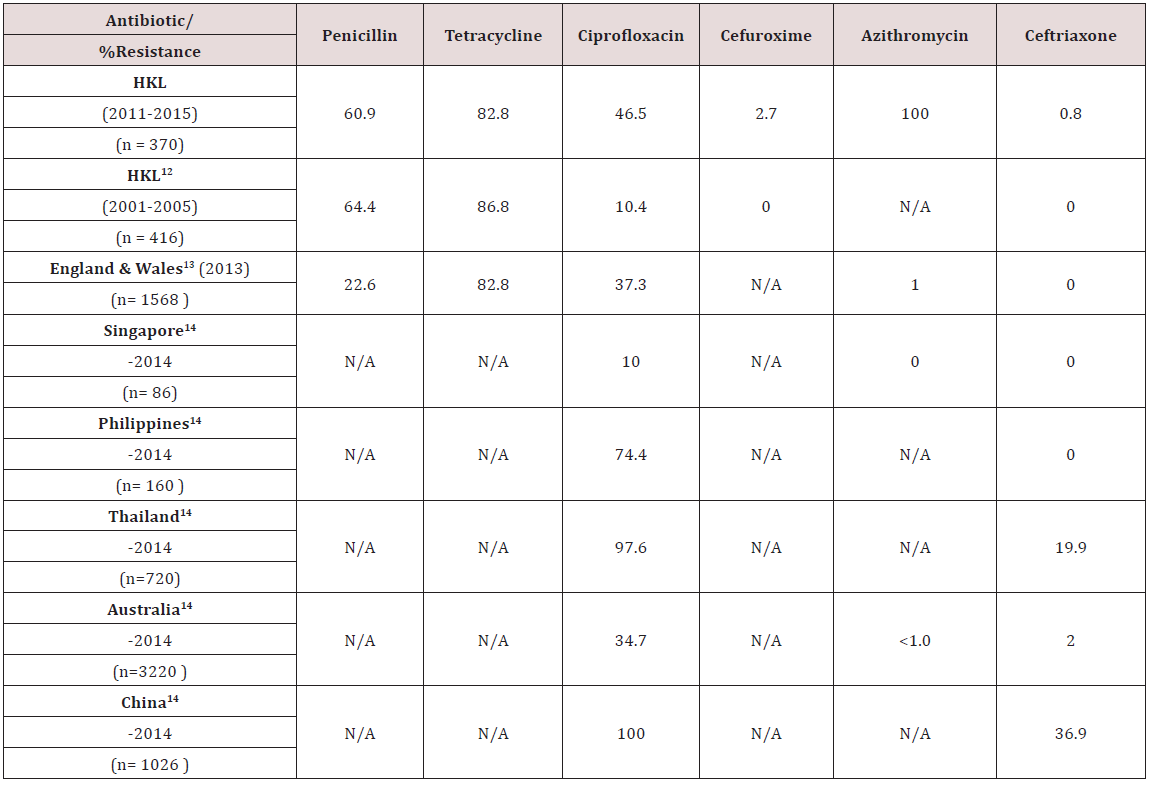
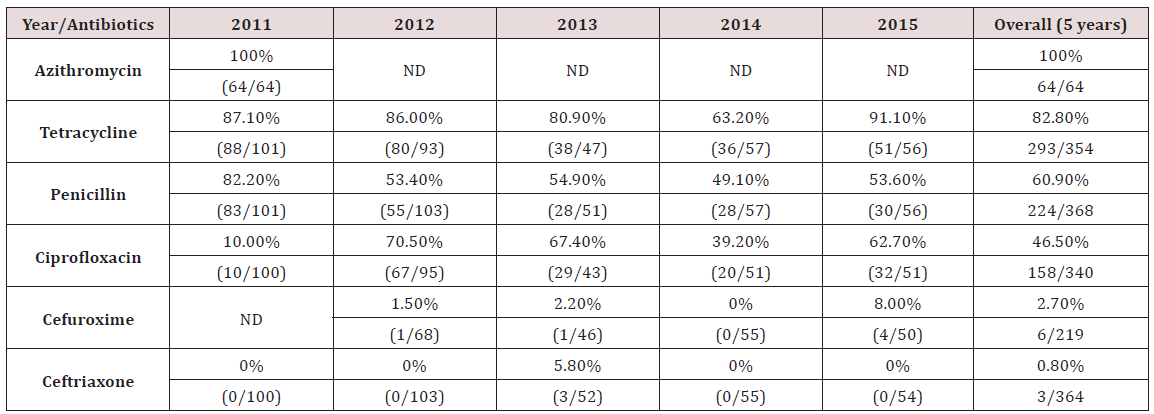
for HIV (Tables 1 & 2). The highest level of resistance detected was
to azithromycin (100%, 64/64), followed by tetracycline (82.8%,
293/354). Resistance to penicillin was noted in 60.9% (224/368)
of all isolates. Both penicillin and tetracycline showed a decreasing
resistance trend from 2011-2014, but increased in 2015. The fourth
commonest antibiotic resistance was to ciprofloxacin at 46.5%
(158/340), followed by cefuroxime 2.7% (6/219). Resistance to
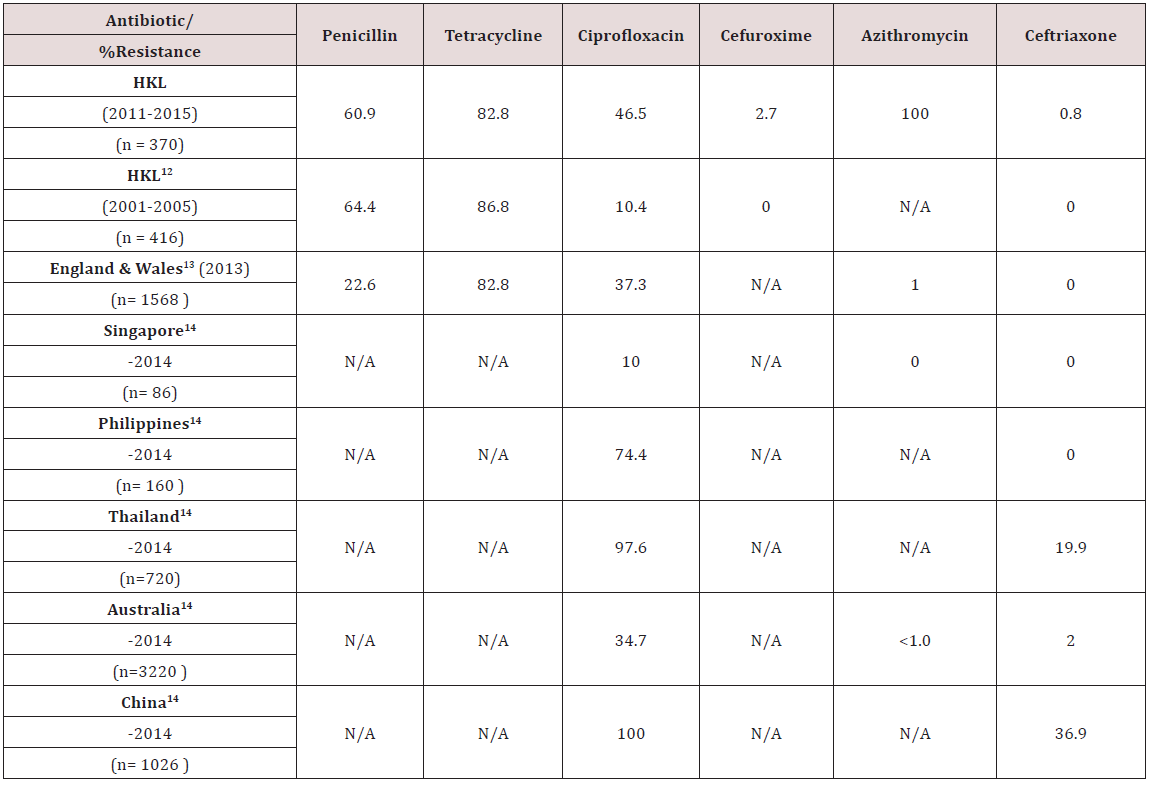
ceftriaxone was 0.8% (3/364), although reviews previously in 2001-2005 showed no resistance [12]. The results were compared
to data obtained from the Gonococcal Resistance to Antimicrobials
Surveillance Programme (GRASP) and WHO (World Health
Organization) Antimicrobial Surveillance Programme [13,14].
Table 1: Demographic characteristics of patients with gonorrhoea.
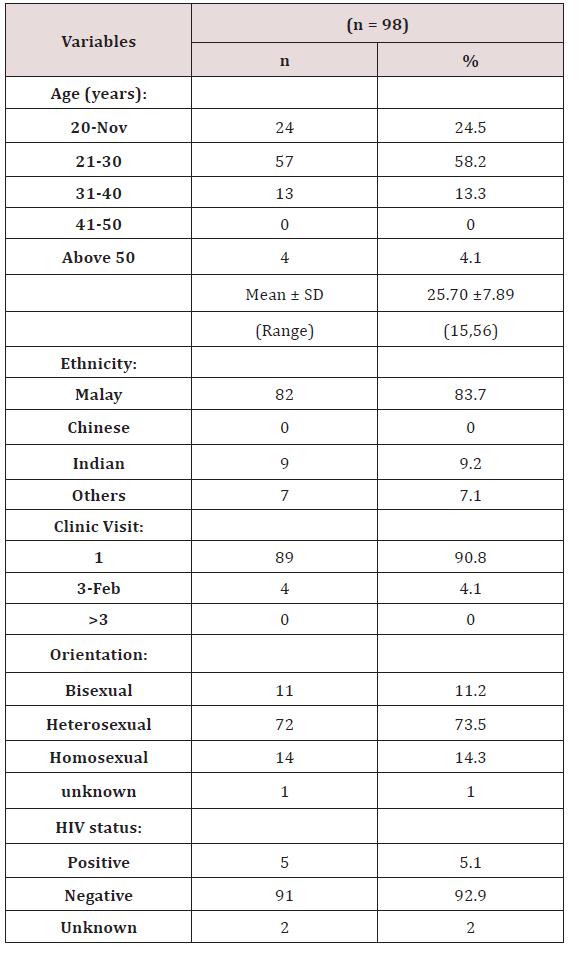
Table 2: Summary of antibiotic resistance pattern of N.gonorrhoeae (2011-2015) in HKL.
Discussion
Azithromycin
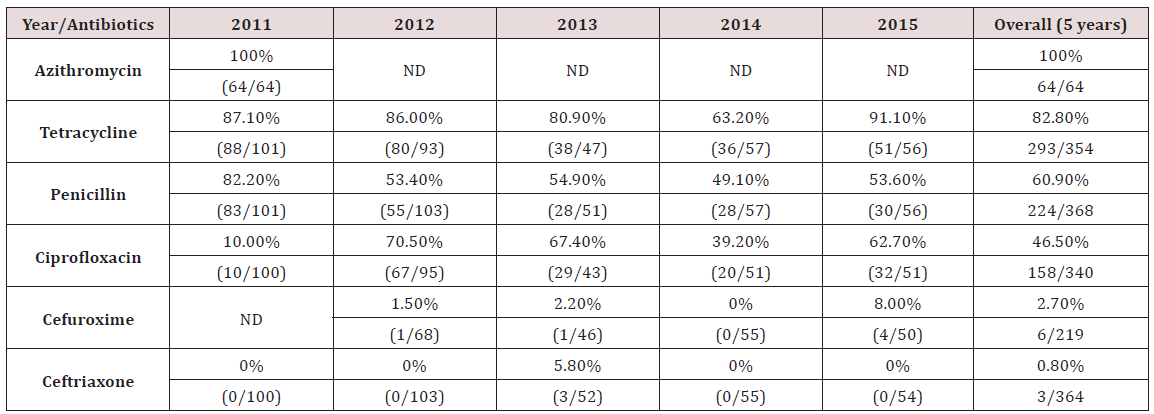
The rate of resistance to Azithromycin in this study was higher
than expected. All 64 samples tested for sensitivity to Azithromycin
showed resistance. In Singapore, no resistance to Azithromycin has
been documented [14]. Similarly in England & Wales and Australia,
the rate of resistance is significantly lower, at 1% or less [13,14]
(Table 3). Studies have indicated concerns for increasing resistance
to Azithromycin, likely due to delay in diagnosis of gonorrhoea and
suboptimal dose of Azithromycin used [15].
Table 3: Comparison of N.gonorrhoeae antibiotic resistance pattern in HKL with other countries.
Tetracycline
The rate of resistance to Tetracycline is high. In our study,
82.8% of N.gonorrhoea isolates were resistant to Tetracycline.
This is slightly lower, compared to an earlier analysis done in HKL
from 2001-2005, where 86.8% of isolates were resistant [12]. The
resistance rates in England & Wales was similar to ours [13] (Table
3). Looking at the trend, there was a reduction in resistance rates
from 87.1% in 2011 to 63.2% in 2014. However, the rate increased
to 91.1% in 2015 (Table 2). In HKL, Doxycycline is sometimes used
to treat non-gonoccocal urethritis but never as primary treatment
for gonorrhoea. Tetracycline has never been used for treating
gonorrhoea in HKL as the resistance is very high. Nevertheless, the
resistance pattern is continuously monitored for epidemiological
purposes.
Penicillin
Since the 1940’s, Penicillin was successfully used to treat
gonorrhoea, but quickly developed decreased sensitivity and
deemed not a suitable treatment after 1970. This can be due to
Penicillinase Producing N.gonorrhoeae (PPNG) or Chromosomal
Mediated Resistance N.gonorrhoeae (CMRNG) [16]. Our study
shows that the rate of N.gonorrhoeae resistance to Penicillin has
reduced, from 82.2% in 2011 to 53.6% in 2015 (Table 2). Compared
to an earlier study done in HKL in 2001-2005, there was a slight
drop in resistance to penicillin in HKL from 64.4% to 60.9% in
2011-2015. However, our resistance rates were much higher
compared to the resistance rate reported in England & Wales of
22.6% (Table 3) [13].
Ciprofloxacin
In the early 1990’s, Ciprofloxacin was widely used especially
by general practitioners to treat gonorrhoea although studies had
already began demonstrating the beginning of reduced sensitivity
to quinolones. The resistance to Ciprofloxacin in HKL showed a
steady increase from 10.0% in 2011 to 62.7% in 2015 (Table 2).
When compared to an earlier review in HKL from the period 2001-
2005, we can see marked increase in resistance to Ciprofloxacin
from 10.4% to 46.5% in 2011-2015 (Table 3). The resistance
rate reported in HKL from 2011-2015 was similar to England
& Wales and Australia, which reported resistance of 37.3% and
34.7% respectively (Table 3) [13,14]. Among the Asian countries,
Singapore reported the lowest resistance to Ciprofloxacin (10.0%)
[14]. Other Asian countries, like the Phillipines, Thailand and China
reported an alarmingly high resistance to Ciprofloxacin, which is
between 74.4%-100% (Table 3) [14].
Cephalosporin–Cefuroxime and Ceftriaxone
Although Cefuroxime is not a recommended treatment for
gonorrhoea, its resistance pattern is monitored for epidemiological
purposes. Our study showed a resistance rate of 2.7% to
Cefuroxime in 2011-2015, whereas an earlier study in 2001-2005
showed no resistance to Cefuroxime (Table 3). Susceptibility
testing for Ceftriaxone use in the treatment of gonorrhoea in HKL
between 2001-2005 indicated no resistance, however, recent
data from 2011-2015 showed a resistance rate of 0.8% (Table 3).
Ceftriaxone is the first line treatment of gonorrhoea in HKL and
clinicians should be aware that we are seeing a small percentage
of resistance in some cases. No resistance was noted in Singapore
and the Phillipines (Table 3) [14]. Resistance rates to Ceftriaxone
in Thailand and China are significantly higher, at 19.9% and 36.9%
respectively (Table 3) [14].
Conclusion
Attempts to treat and control gonorrhoea are compromised by
the emergence and spread of antibiotic-resistant N.gonorrhoeae.
WHO expert committee has recommended that treatment regimen
be altered once resistance to a particular antibiotic reaches 5%.
High rates of resistance to Penicillin and Tetracycline have been
documented in HKL and in the Western Pacific region. Within
15 years, a marked increase in Ciprofloxacin resistance (10% to
46.5%) is evident. Resistance to Cefuroxime and Ceftriaxone was
discovered, which was not found in the previous study. Ceftriaxone
remains the first line antibiotic in treating gonorrhoea in HKL, and
clinicians need to be aware of the small percentage of resistance
detected to Ceftriaxone.
To Read More Click on Below Link
https://lupinepublishers.com/research-and-reviews-journal/fulltext/antibiotic-resistance-pattern-of-nesseria-gonorrhoea-at-the-genitourinary-medicine-clinic-hospital-kuala-lumpur-malaysia.ID.000124.php
For more
Lupine Publishers Open Access Publishers Please Visit our Website
https://lupinepublishersgroup.com/
For More
Medical Care Research and Review Articles click on below link
https://lupinepublishers.com/research-and-reviews-journal/
To Know more about
Open Access Publishers please click on
Lupine Publishers